How to Prevent Hypoglycemia and Live Well with Diabetes
Welcome! Are you here to learn more about hypoglycemia? Whether you’re a patient living with diabetes yourself, a caregiver/loved one of a diabetes patient—or just someone who wants to know more about diabetes and hypoglycemia risks—we are glad you’re willing to take some time out of your busy day to learn more about this condition.
On this site, you’ll discover how to manage your hypoglycemia risk and live well with diabetes, pre-diabetes, or other conditions which may place you or your loved ones at risk for developing hypoglycemia.
Hypoglycemia Education










 Shakiness,
dizziness
Shakiness,
dizziness
 Agitation,
nervousness
Agitation,
nervousness
 Blurry vision
Blurry vision
 Heart
palpitations, sweating
Heart
palpitations, sweating
 Tingling feeling
in fingers, hands or face/lips
Tingling feeling
in fingers, hands or face/lips
 Unusual behavior,
slurred speech
Unusual behavior,
slurred speech
 Fainting
Fainting  Generally feeling
unwell or “off”
Generally feeling
unwell or “off”

































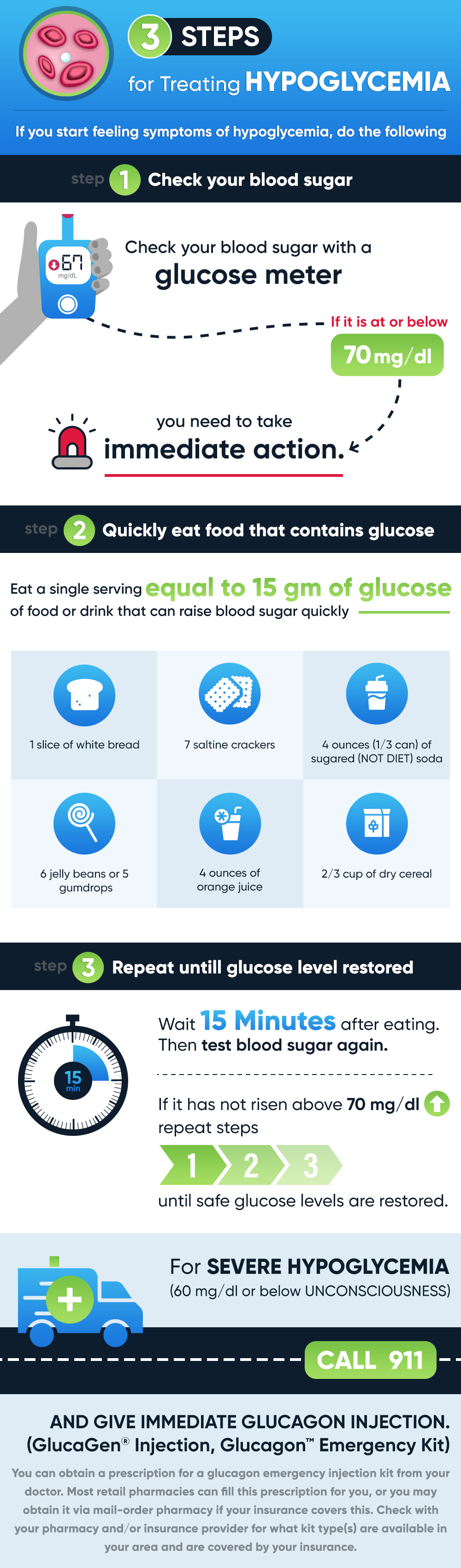
 How Do You Treat Hypoglycemia?
How Do You Treat Hypoglycemia?